Shadow People Encounters: What the Medical Record Certifies
What can today’s medical record certify about shadow people encounters, and where does it stop short of certifying entities at all?
This article treats shadow-figure reports as a documentation problem, using only institutional health and academic records that remain citable.
- Visual hallucination: seeing something not actually present, linked to medical or mental health causes
- Sleep paralysis described as REM-related processes intruding into waking consciousness
- Sleep-paralysis-consistent experiences interpreted through local folklore frameworks
- Severe sleep deprivation documented as progressing from misperceptions to hallucinations and other psychosis-like symptoms
- Nyctalopia tied to impaired dark adaptation, with rod-cell association in night vision physiology
These points define the stable edge of what this source set can certify, before it runs into missing scale estimates and missing triage guidance.
Evidence gate: the Sleep Foundation sleep paralysis explainer page at /sleep-demon
A reader opens a Sleep Foundation page whose address ends in /parasomnias/sleep-demon. The page presents itself as a plain-language explainer for sleep paralysis experiences.
In the section describing reported content, the text includes a sense of presence. It also uses language consistent with feeling watched during the episode.
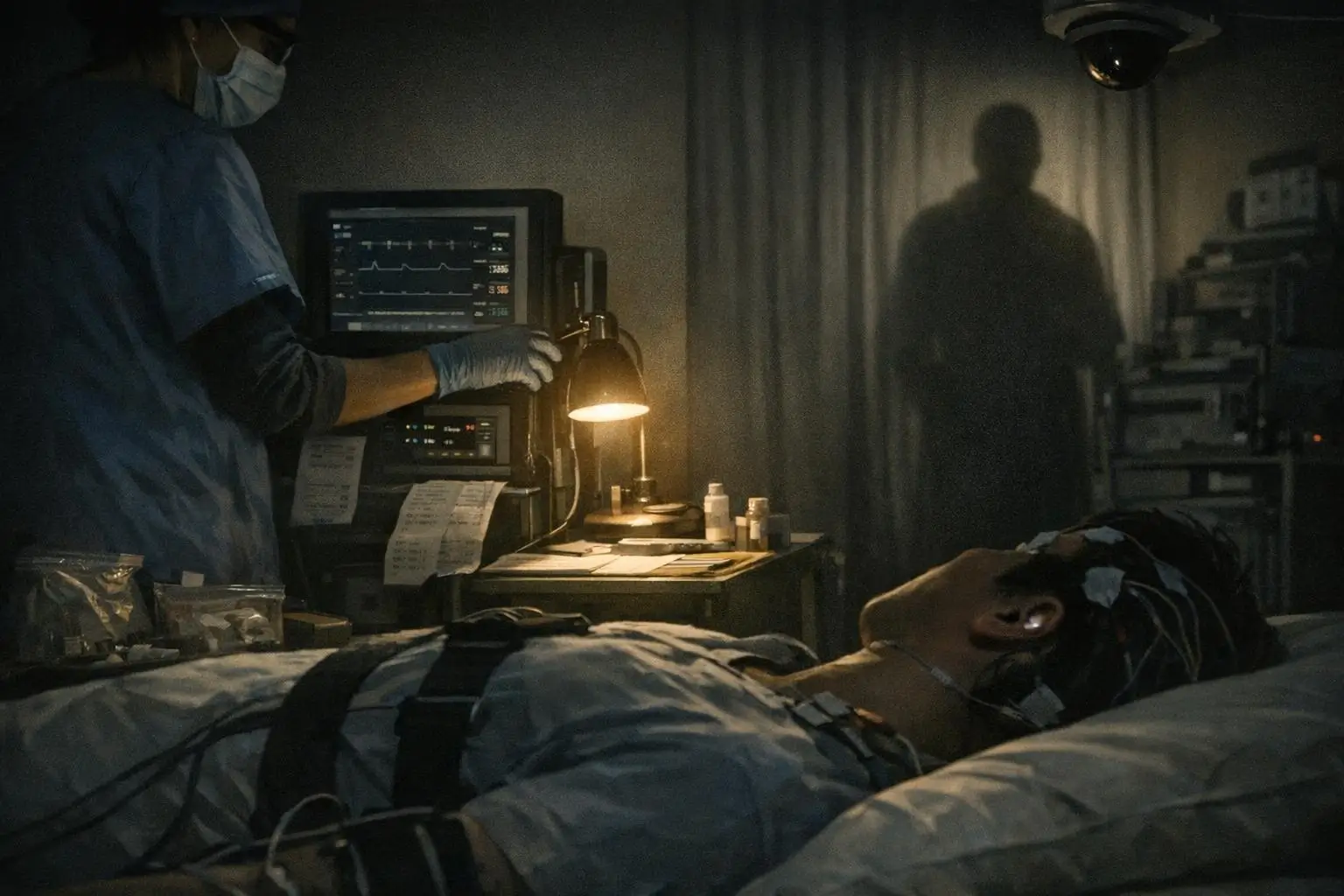
The page includes the phrase ‘shadowy, human-like figures’ as something people report seeing. The record, in this format, preserves the phrase without treating it as external confirmation.
The same passage groups bodily sensations with perceptual content, including chest pressure. The document frames these as reported features during the paralysis state.
In this single page, the key point is not an entity claim. The key point is that an institutional health explainer uses a figure-like description as part of the sleep paralysis report pattern.
The page does not provide population totals or a rule for when a person should seek urgent eye evaluation. It functions as a public-facing description rather than an individualized medical workup.[1]
This evidence gate can certify that figure-like language exists inside an institutional description of sleep paralysis. It does not certify frequency, cause, or meaning in any individual report.
What the record means by seeing something: a bounded definition of visual hallucination
One stable anchor in this archive is definitional. A visual hallucination is described as seeing something that is not actually present.
This framing keeps the category clinical rather than supernatural. The record allows the statement that visual hallucinations can be associated with medical or mental health causes.
This definition does not, by itself, classify any shadow-figure report as a hallucination. It only sets the allowable boundary for language when a person describes seeing something that is not there.[2]
The mechanism phrase the academic record does preserve: REM intrusion into waking consciousness
A second anchor is mechanistic, but narrow. A PubMed-indexed description frames sleep paralysis as an anomalous intrusion of REM processes into waking consciousness.
That phrase can support careful wording about state-mixing between sleep and wake. It cannot, from this excerpt alone, certify why one person reports a silhouette while another reports something else.
The record also does not supply a step-by-step neurocognitive pathway in this source set. What it preserves is permission to speak about REM-related processes intruding into waking experience in sleep paralysis contexts.[3]
Why the same experience can be narrated as an entity: the sleep paralysis and folklore linkage
A separate peer-reviewed line addresses interpretation rather than physiology. It documents that experiences consistent with sleep paralysis have been interpreted through local folklore frameworks.
This gives a way to describe why entity-like narratives can recur across cultures without treating any one narrative as verified. It is an interpretation layer attached to a reported experience layer.
The archive still cannot supply primary ethnographic examples from specific communities here. The validated set does not include university press or primary field documentation, so the cross-cultural claim stays high-level.[4]

Another non-paranormal pathway the record does document: severe sleep deprivation progression
Not all shadow-figure talk is anchored to sleep paralysis in the surviving record. A peer-reviewed review describes prolonged sleep deprivation as progressing from misperceptions to hallucinations and other psychosis-like symptoms with increasing time awake.
This provides a documented escalation pattern that can overlap with figure-like reports in general conversation. It does not certify that any specific silhouette report was caused by sleep loss.
The validated material also does not provide a threshold in hours or a clinical decision rule. What remains stable is the direction of change described in the review: misperception can progress toward hallucination under severe deprivation.[5]
Peripheral visual effects with documented labels: scintillating scotomas and visual migraine
Some reports focus on peripheral visual disturbance rather than a bedroom episode with paralysis. In that space, the archive includes a specific medical term: scintillating scotomas.
Scintillating scotomas are described as temporary blind spots with shimmering or sparkling effects, commonly associated with migraine. A related patient-education framing discusses visual migraine phenomena in a neuro-ophthalmology context.
This source set does not certify that migraine-linked visual effects appear as a human-like silhouette. It only permits naming one documented pattern of unusual visual perception that can occur, including in peripheral experience.[6]
Low-light perception constraints the record can name: nyctalopia and dark adaptation
Some silhouette reports are tied to dim rooms, night driving, or low-light transitions. The archive can support only one limited move here: naming dark adaptation physiology and a defined impairment label.
Nyctalopia is described as an impaired ability to adapt from lightness to darkness. In that medical reference framing, rod cells are the principal cell type associated with nyctalopia.
This does not certify that a person with normal night vision cannot misperceive shapes in the dark. It only fixes a documented concept for why low-light perception can be constrained in some conditions.[7]
Where the archive breaks: scale, triage, and culturally specific detail
Public framing often treats shadow people encounters as a global paranormal mystery. This validated record set cannot quantify that scale because it contains no tier-1 prevalence estimates for sleep paralysis, misperceptions, or hallucinations in healthy populations.
A second break is practical. The archive does not include institutional ophthalmology guidance on urgent versus benign causes of sudden peripheral shadows, so it cannot document warning signs or decision rules.
A third break is cultural specificity. The record supports the existence of folklore interpretation frameworks, but it does not include primary ethnographic documentation needed to name specific narratives, sites, or community-level patterns.
These breaks matter because they limit what can be responsibly said. They also define the next documentary targets: prevalence studies, ophthalmology triage guidance, and primary ethnographic sources that meet the same evidence policy.
Documented incompleteness: what can be certified about shadow figures, and what cannot
The record in this article can certify that sleep paralysis descriptions include reported presence and figure-like perceptions, including ‘shadowy, human-like figures’. It can also certify that an academic mechanism phrase exists: REM-related processes intruding into waking consciousness.
The same archive can certify that prolonged sleep deprivation is documented as progressing from misperceptions to hallucinations and other psychosis-like symptoms. It can certify that some peripheral visual disturbances have medical labels, including scintillating scotomas linked with migraine, and that low-light adaptation limits are documented under nyctalopia and rod-cell physiology.
What it cannot certify is the existence of dark entities, interdimensional beings, or any other external agent behind these reports. It also cannot certify how common the experience is, or when a peripheral shadow report is medically urgent, because those documents are not present here.
If a person is distressed and wants a documented help route for treatment referral and information, the archive does include one official service description.[8]
FAQs (Decoded)
Does an institutional health source explicitly mention shadowy figures during sleep paralysis?
Yes. A Sleep Foundation sleep paralysis explainer includes reported content such as a sense of presence and ‘shadowy, human-like figures’ within that context. Source: Sleep Foundation, sleep paralysis explainer page.
Does this record prove that shadow people are real entities?
No. The validated sources used here document reported experiences, definitions, and mechanisms, but they do not certify external entities. Source: WebMD, visual hallucination definition and clinical framing.
What mechanism language is documented for sleep paralysis in this archive?
The source set preserves a peer-reviewed phrasing that sleep paralysis involves an anomalous intrusion of REM processes into waking consciousness. Source: PubMed, sleep paralysis REM-intrusion record excerpt.
How does folklore enter the record without validating supernatural claims?
The archive includes a peer-reviewed discussion that sleep-paralysis-consistent experiences are interpreted through local folklore frameworks, which can shape recurring entity narratives without confirming them. Source: PubMed Central, sleep paralysis and folklore article.
Can sleep deprivation be linked to hallucination-like experiences in the validated material?
Yes. A peer-reviewed review documents a progression under prolonged sleep deprivation from misperceptions to hallucinations and other psychosis-like symptoms with increasing time awake. Source: PubMed Central, severe sleep deprivation review.
What is a scintillating scotoma in the sources used here?
It is described as a temporary blind spot with shimmering or sparkling visual effects, commonly associated with migraine. Source: Cleveland Clinic, scintillating scotoma symptom page.
Is there a documented support resource included if someone feels overwhelmed by these experiences?
Yes. The archive includes a government resource describing SAMHSA’s free, confidential, 24/7 National Helpline for treatment referral and information. Source: SAMHSA, National Helpline service description.
For more paranormal case files, explore the archive. The ghosts and demons files contain related documentation. Additional entries include haunted places case files and poltergeist activity case files.
Sources Consulted
- Sleep Foundation, sleep paralysis explainer page describing reported presence and shadowy figures. sleepfoundation.org, accessed 2025-02-17
- WebMD, patient-facing explanation of seeing things and visual hallucinations. webmd.com, accessed 2025-02-10
- PubMed, record excerpt describing sleep paralysis as anomalous intrusion of REM processes into waking consciousness. pubmed.ncbi.nlm.nih.gov, accessed 2025-02-03
- PubMed Central, peer-reviewed article on sleep paralysis and folklore interpretations. pmc.ncbi.nlm.nih.gov, accessed 2025-01-27
- PubMed Central, peer-reviewed review on severe sleep deprivation symptom progression. pmc.ncbi.nlm.nih.gov, accessed 2025-01-20
- Cleveland Clinic, scintillating scotoma symptom definition and migraine association; Brigham and Women’s Hospital, visual migraine patient education. my.clevelandclinic.org, accessed 2025-01-13
- NCBI Bookshelf, nyctalopia definition and rod-cell association in night vision physiology. ncbi.nlm.nih.gov, accessed 2025-01-06
- SAMHSA, National Helpline service description. samhsa.gov, accessed 2024-12-30

A Living Archive
This project is never complete. History is a fluid signal, often distorted by those who record it. We are constantly updating these files as new information is declassified or discovered.


